The H. Pylori Controversy: Does it Really Cause Heartburn, Acid Reflux, and GERD?
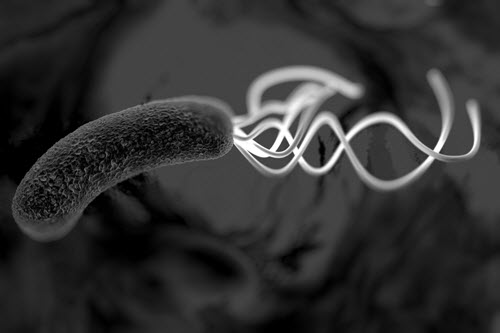
This little bacteria…
It infects more than 50% of the world’s population.
Flip a coin and that’s the probability you have it living inside your GI tract right now.
But is it hurting you? Or maybe, just maybe, the infection is helping you…
There’s evidence linking this infection to ulcers and stomach cancer. But then again, there’s evidence it may play an important role in your immune system and gut flora.
This is the controversy of H. pylori.
And this is what we’re going to dive into in this article.
How Two Hardcore Scientists Discovered H. Pylori
H. pylori is a bacteria. It’s full name is Helicobacter pylori.
It was unknown until two hardcore scientists discovered it in 1982.
See, back then it was commonly believed that stomach ulcers were just a byproduct of stress. But these two Australian scientists, Barry Marshall and Robin Warren, didn’t believe that.
Marshall and Warren discovered a bacteria (H. pylori) and decided to take biopsies of patients with stomach ulcers and gastritis. They formulated the hypothesis that H. pylori was actually the cause of such G.I. disorders.
The problem was that they needed a way to prove it. Unable to run trials on mice (H. pylori can’t infect mice) and unable to get approval for human studies… Marshall infected himself with H. pylori and, after developing precursory ulcer symptoms, biopsied his stomach and found the suspected culprit. He proceeded to treat himself with antibiotics to get rid of the infection and made a full recovery.
That’s dedication to science!
The Evidence Against H. Pylori
This is where things start to get interesting. Since 1982, this infection has been studied extensively beyond stomach ulcers and gastritis… and these days it’s also linked to things like:
- NSAID gastropathy (inflammation due to use of NSAIDs)
- Gastric carcinoma (stomach cancer)
- Lymphoma (cancer/tumors in the lymphatic system)
…not to mention disorders outside of the G.I. tract like: ischemic heart disease, ischemic cerebrovascular disorders, rosacea, raynaud’s syndrome, food allergy, Vitamin B12 deficiency, and open-angle glaucoma. It’s also been noted that H. pylori infections can increase inflammation throughout the entire body.
That’s a whole lot of bad stuff. So far, H. pylori has a bad reputation.
The evidence gets even worse, just look at how prevalent H. pylori is in the following conditions:
- 80-100% of those with duodenal ulcers
- 70% of people with gastric ulcers
And yet, we aren’t totally sure how it’s spread. We do know that if you live with someone with an H. pylori infection, your chances of developing an infection are much greater. Whether it’s passed through saliva, fecal matter, food, or animals is still up for debate.
Also, one school of thought is that these infections could start in early childhood and it’s actually your genetics and lifestyle choices that dictate whether it results in something harmful like gastritis, ulcers, or stomach cancer.
Those with low stomach acid may be at a greater risk, too.
Stomach acid not only helps to digest food, but it also prevents infections. As you get older, your stomach acid levels can decrease (a condition called hypochlorhydria) and it may be why the population over 50 has a higher prevalence of infection.
Not only that, but H. pylori can suppress stomach acid levels, making the cycle even worse.
According to the Textbook of Functional Medicine, low stomach acid predisposes one to the growth of H. pylori and is also linked to SIBO and inadequate Vitamin B12 absorption. It’s also noted that low levels of vitamin C, and vitamin E in gastric fluids promote the growth of H. pylori. And while there aren’t decisive studies showing that H. pylori is the direct cause of heartburn and acid reflux, there is an implied association there.
It’s not looking good for this bacteria so far. Here’s how to tell if you have it living inside you right now.
Signs and Symptoms You Have H. Pylori
The data suggests that 85% of people infected with H. pylori never experience symptoms, but here’s a few clues this is something you might have right now:
- Burning or ache in the abdominal region – worse on an empty stomach
- Nausea
- Loss of appetite
- Burping
- Bloating
- Weightloss
Of course, this list of symptoms could be from many different root causes, so it’s important to make sure you get tested to know for sure. The following tests are ways to find out if your symptoms may be caused by H. pylori:
- Breath test (C urea)
- Serology
- Blood test for H. pylori antibodies
- Stool antigen test (like the BioHealth 401H)
- Intestinal biopsy (histology, culture, rapid urease test, PCR)
Like any modern day medical testing, each of these has its own drawbacks with regards to how invasive it is, reliability and sensitivity, and the cost.
Another complication is there doesn’t seem to be a “gold standard” test that exists, as this article puts it, A combination of methods tested against one another may be the best approach to confirm the presence (or absence) of H. pylori infection.
Polymerase chain reaction (PCR) from an intestinal biopsy seems to be the most sensitive and specific, but it’s pretty invasive because it requires an instrument to be inserted down your throat. And there’s a debate about the tissue selection. It’s possible (not sure how much yet) for the selected tissue to be negative but surrounding areas positive (they just weren’t sampled).
In our experience (and our own battle with H. pylori), the Stool antigen test from a BioHealth 401H has worked well.
So You Have H. Pylori – How Do You Treat It?
This is where the controversy comes in…
Most doctors just treat it if there’s a diagnosed ulcer, but you can still have an infection, and not a diagnosable ulcer. It’s a little concerning given the evidence that H. pylori infections are linked to greater chances of developing other disorders/diseases aside from stomach cancer, chronic gastritis, and ulcers.
But if you test positive for H. pylori… but you don’t have any symptoms – is treatment worth the risk?
There are some natural H. pylori remedies out there, like bismuth subcitrate, deglycyrrhizinated licorice, and mastic gum resin. But most H. pylori infections in the modern medicine setting are primarily treated with a powerful cocktail of antibiotics.
It’s usually a combination of antibiotics, like amoxicillin, lansoprazole, and/or clarithromycin along with an antacid regimen (usually some PPI). While this can and does work, antibiotics as a viable means for treating H. pylori may not be so effective in the future.
Plus, if you follow our work, you know that a healthy gut flora is critical to a happy gut, so a heavy dose antibiotic protocol isn’t going to support that. In fact, one study actually linked antibiotic eradication of H. pylori to fungal growth in gut mucosa, which actually makes sense. You are literally trying to destroy a bacteria, and sadly the antibiotics aren’t selective for just one species of bacteria – you’re taking out the good guys, too.
And that’s where things get tricky.
The gut bacteria isn’t so black and white. There are some bacteria that are symbiotic (they help us we help them), some that are pathogenic (they only harm us), but then there are some more middle of the road. It’s currently thought that these bugs don’t t really help us or hurt us, depending on the circumstances.
But while evidence on specific strains of bacteria being good or bad is sorted out, what is accepted is that you want a large diversity of bacterial species in the gut. And heavy antibiotic therapy definitely reduces the number of species in the short-run and might be an issue in the long-run.
So Is H. Pylori Good or Bad?
Up until this point, you might be thinking H. pylori is definitely a bad guy and should be killed off. But that’s not the full story…
One of our mentors, Chris Kresser, has a great talk on this (you can check it out here) – and he uses H. pylori as an example of a middle of the road kind. In the talk, he mentions this one study where H. pylori was actually shown to help prevent against asthma in animals, but only if it was contracted early enough.
H. pylori infections introduced later in life are associated with greater amounts of inflammation and greater risk of stomach cancer. But it’s possible the earlier in life H. pylori is introduced, the more it serves as a protective factor. Timing and bacterial cross-talk, though minimally understood, are proving to be critical and fascinating factors in health.
During Kresser’s talk, he reviews a study which focuses on people from an area called Sardinia, where the population was infected with Malaria (usually a super bad infection). Those with a trait for sickle cell anemia were able to live with the infection without any problems. In the 1950s, there was a movement to eradicate Malaria from this island. Soon after it was completely eradicated, the onset of autoimmune disease, in the form of type 1 diabetes and multiple sclerosis, spiked through the roof. The theory is that the Malaria infection was doing more than ever thought – that it was affecting and modulating its host’s immune systems, preventing them from getting these other diseases.
When this same theory is applied to chronic infections, it goes like this: if you get a chronic infection early enough (like the Malaria example), then your immune system development and function are governed and influenced by it and it could begin to help you and removing it may cause unknown and detrimental effects.
Kresser says it like this: “Imagine you’re standing and facing someone, and you both have your hands out and you’re leaning into each other, and all of a sudden somebody steps away, you’re going to fall down.”
So the bottom line: Just because you have an H. pylori infection doesn’t mean you will develop gastritis, cancer or an ulcer… and the symptoms of heartburn, GERD, and acid reflux.
You may not even show signs or symptoms, and that may be a good thing. It may be how it’s supposed to be… unless you have ulcers, or in our opinion, any other digestive related problems.
Our current point of view is that if you’re struggling with ulcers, gastritis, heartburn, GERD, acid reflux, or other GI symptoms AND you test positive for H. pylori… it’s probably a good idea to treat it.
The most common reason being: H. pylori has been shown to suppress stomach acid, which you need to fix to finally get rid of the symptoms of heartburn once and for all…
Not to mention properly digest and absorb the nutrients from your food.
How to Treat the Root Cause of Heartburn
Contrary to what you might have been told, there are 7 root causes of heartburn, acid reflux or GERD.
And it starts with understanding that the main issue isn’t that you aren’t producing too much acid. Instead, it’s actually the opposite – you’re likely producing too little acid.
The root cause of this low stomach acid can be multifactorial, but we do know that H. pylori infections can play a huge role.
And after overcoming this issue myself and helping 100s like me, we decided to do a dedicated 3-hour presentation on how to overcome heartburn naturally.
I urge you to check it out here: http://heartburnhelp.scdlifestyle.com
During this presentation, we’ll help you understand the most important short-term and long-term strategies to start naturally taking control of this condition.
What we cover during the ‘Getting Rid of Heartburn’ presentation:
- The 3-step “rest, repair, and reset” to unlock your body’s natural ability to heal from the damage of years of antacid pills
- How to break free of the dependence on pills holding you back from life-changing restoration of healthy stomach acid levels
- The sneaky little root causes that keep your stomach acid low – even after you’ve stopped the pills – and keep the cycle of heartburn raging
- What you MUST be avoiding in order for your stomach to heal (or the symptoms will come right back)
- The step-by-step process we’ve used to naturally get rid of heartburn and restore normal stomach acid levels (even if they’ve been on PPIs for 20 years)
- Why food is critical – and not so critical – for your long-term success getting rid of heartburn
- A simple method for cultivating normal stomach acid levels that trigger great digestion… even for some foods you couldn’t tolerate before
- Specific supplements to take – and other ones to avoid – on your road to healing the stomach and fixing your heartburn
- Why H. pylori, SIBO, Hormones, and other root causes could be the REAL reason you’re still suffering from heartburn, even though you’ve done everything else right
- Plus, much more…
Click here to get this life-saving information: http://heartburnhelp.scdlifestyle.com
– Jordan
Did You Like this Article?
Subscribe to our newsletter to receive email notifications, some ways to find relief, and next steps.
